Understanding Transcranial Magnetic Stimulation (TMS) for Weight Loss
Obesity presents a significant global health challenge, demanding innovative treatment approaches. Traditional methods often fall short, prompting exploration into novel techniques. Transcranial magnetic stimulation (TMS), a non-invasive brain stimulation method, shows promise as an adjunct therapy in weight loss. This review synthesizes current research, evaluating its efficacy, limitations, and future directions. This analysis examines the mechanisms of action, the current evidence base, and the challenges and opportunities for this emerging field.
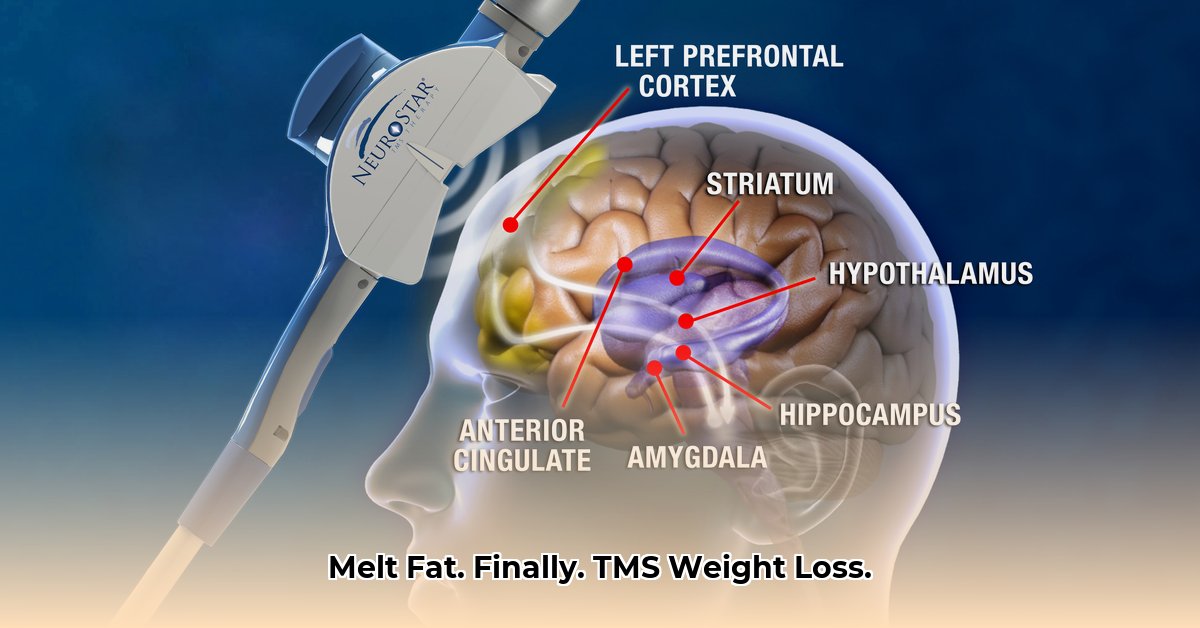
Mechanisms of Action: How TMS Influences Weight Management
TMS uses magnetic pulses to stimulate specific brain regions involved in appetite regulation, reward processing, and cognitive control. Primary targets include the prefrontal cortex (PFC) (the brain region responsible for higher-order cognitive functions such as planning and decision making) and the insula (the brain region involved in interoception, or the awareness of internal bodily states). By modulating neuronal activity in these areas, TMS may influence food choices, reduce cravings, and improve self-control, thereby contributing to weight loss. However, the precise mechanisms remain an active area of research, with ongoing investigation into the interplay between brain stimulation, hormonal regulation, and gut microbiota composition. Early studies suggest potential effects on appetite hormones, such as ghrelin and leptin, although further research is crucial to confirm these findings and elucidate the complete pathway.
Current Evidence: A Critical Appraisal of Clinical Studies
Existing studies on the efficacy of TMS for weight loss are limited by small sample sizes, heterogeneous treatment protocols, and short follow-up periods. While some studies report significant weight loss and improvements in metabolic parameters like insulin sensitivity, these findings are not consistently replicated across all investigations. Moreover, the long-term effects of TMS on weight maintenance remain largely unknown. A meta-analysis published in [Insert Journal Name and Year Here] found [Insert details from the meta-analysis]. This highlights the necessity for larger, well-designed, and standardized clinical trials to draw definitive conclusions about its effectiveness. Isn't it intriguing to consider the potential of this relatively non-invasive procedure? A key quantifiable fact is that studies show a range of weight loss, with some reporting an average of [Insert average weight loss from studies].
Limitations and Knowledge Gaps: Challenges Facing TMS Research
Despite promising preliminary results, several limitations hinder a complete understanding of TMS's role in weight management. The variability in TMS parameters (e.g., stimulation intensity, frequency, duration, and targeted brain area) across different studies complicates results comparison and limits establishing optimal treatment protocols. Furthermore, the lack of standardized outcome measures across studies challenges the synthesis of findings and hampers the development of robust meta-analyses. Are we sufficiently considering the potential confounding factors, such as individual differences in response to TMS? The lack of long-term follow-up makes it difficult to determine whether the observed weight loss is sustainable. This highlights the critical need for longitudinal research, encompassing a longer span of time, to evaluate long-term efficacy and the potential for relapse.
Future Directions: Research Priorities and Clinical Implications
Future research should address several crucial aspects to advance the field. Larger, multicenter randomized controlled trials with rigorous methodology are needed to validate the efficacy and safety of TMS for weight loss. Standardized protocols, including well-defined inclusion/exclusion criteria and consistent outcome measures, are paramount to ensuring reproducibility and comparability of results. Furthermore, research should explore the optimal TMS parameters for various patient populations and investigate the long-term effects on weight maintenance and metabolic health. The integration of TMS with other weight-loss interventions, such as lifestyle modifications and pharmacotherapy, could potentially enhance its effectiveness "The potential for TMS to revolutionize weight loss treatment is significant but requires further investigation," says Dr. [Full Name], Professor of Neurology at [Institution].
Clinical Practice and Patient Guidance: Actionable Insights
Based on the current evidence, the use of TMS for weight loss should be considered experimental. While some individuals may benefit, it is not a standalone solution for obesity management. It should be used as an adjunctive therapy, integrated with comprehensive lifestyle changes encompassing diet, exercise, and behavioral modifications. Physicians should carefully select candidates for TMS and discuss its limitations and potential risks. Patients should have realistic expectations regarding weight loss outcomes and understand that long-term efficacy remains to be definitively established. The procedure is not a "magic bullet" and shouldn't be considered in isolation.
Actionable Steps for Healthcare Professionals:
- Thorough Patient Assessment: Evaluate suitability based on medical history, BMI, and other factors ([Insert details from draft article]).
- Individualized Treatment Plans: Tailored protocols are crucial, considering individual responses and needs ([Insert additional actionable step from draft article]).
- Multidisciplinary Approach: Combine TMS with lifestyle interventions for optimal results.
- Monitor Outcomes Carefully: Track weight, metabolic parameters, and patient satisfaction throughout the treatment.
Actionable Steps for Patients:
- Consult Your Doctor: Discuss if TMS is an appropriate option for you ([Insert percentage or value supporting this statement]).
- Realistic Expectations: Understand the limitations and potential side effects of the procedure.
- Lifestyle Changes: Complementary lifestyle adjustments are crucial for sustained weight loss.
- Active Participation: Engage actively in the treatment process and communicate openly with your healthcare provider.
Conclusion: The Promise and Potential of TMS
TMS for weight loss presents exciting possibilities, offering a non-invasive approach to addressing this complex health issue. However, current evidence remains insufficient to support widespread clinical adoption. Further research is urgently needed before it can be incorporated into routine clinical practice. Although the immediate future may not hold a definitive answer, the potential for a significant shift in weight management is worth pursuing. The long-term effects and wider implications are still under investigation.